Piloting Whole Genome Sequencing in Newborns in the United Kingdom
Genomics England is preparing to launch a pilot programme to test the use of genomics in newborn screening. I spoke with Dr. David Bick, Principal Clinician, Newborn Genomes Programme, about the programme’s aims and structure.
Interview with Dr. David Bick
How did the idea for Genomics England’s Newborn Genomes Programme come about?
The United Kingdom (UK) has a long history of investment and interest in healthcare and genetics. Whole genome testing is not a new or radical idea in the UK, but one that has been talked about for years. The UK government is seeking to understand how it wants to position itself with respect to newborn screening by genomics and these conversations have resulted in the following developments:
About four years ago, Sally Davies, Chief Medical Officer for England at the time, hosted a conference where experts from around the world debated using genomics in a newborn setting. The outcome of this meeting was the recommendation for a pilot program that would examine the possibility of using whole genome sequencing as an adjunct to the current newborn screening programme in the UK. In 2021, the Ministry of Health, announced the launch of a pilot program that would sequence the genome of 100,000 newborns.
What are the benefits of whole genome sequencing in newborns?
Current newborn screening (NBS) is mainly done using analyte testing, by measuring a chemical substance in the blood to indicate whether the child is likely to have a condition. Adding a new analyte test for a new condition to NBS panels is a lengthy process; it requires proving that each screening process can reliably capture most newborns with a condition (appropriate sensitivity and specificity), ensuring that local laboratories have the adequate expertise and technology to perform the screening and that there are enough resources to undertake this test for all newborns, etc. For example, in the United States, it can take 7-9 years to add a new condition to a NBS panel and States currently test for about 50 conditions. By contrast, we have a database with more than 700 treatable conditions that appear in childhood that can be reliably detected through genome screening (see rx-genes.com for a list of these conditions).
So, given the delays and barriers to analyte testing, maybe we need to consider genetic testing as an alternate technology. Using genome sequencing, we could detect many more conditions through one process and one technology.
It is important to clarify that while our programme will sequence all genes, our review of genetic abnormalities remains targeted to pre-defined conditions that can be identified through clear mutations in the genome. When you look at DNA code, you find three types of variants (changes): 1) pathogenic variants, which cause disorders; 2) benign variants, which do not affect the body’s function; and 3) variants of uncertain significance (or VUS), of which we are not exactly sure of the outcome. We do not want to test for conditions that are sufficiently variable that even with a pathogenic variant, we would not know how seriously it would manifest in the child – and we definitely do not want to call parents and say that their child has a problem, but we do not know what it means. So, for our programme, we will only be looking for conditions with clearly identified pathogenic variants.
We anticipate we will end up testing for about 300 to 400 of the 700+ conditions identified in the database, including those already part of the newborn screening programme, but this will be determined over the coming months as part of the pilot programme.
How is the pilot being organized?
We are building the pilot with the involvement of various stakeholders, including:
Parents – parents need to think the programme is a good idea, particularly as we plan to follow up with all participating families (whether we found pathogenic variants or not) for many years to understand the evolution of conditions in children and the parents’ experience in the programme.
Physicians – physicians also need to think the programme is a good idea and a valuable use of their time as they will deliver the results to families. In addition, as this is only a screening test, every confirmed pathogenic variant will need to be confirmed through a follow-up diagnostic test as part of routine medical care.
National Health System (NHS) – this programme needs to be economically worthwhile for the UK government; we, therefore, need to prepare an economic analysis that compares the cost of the programme, plus the cost of treating the children identified through the programme, to the cost of failing to treat affected children with timely intervention.
The programme is being developed in a stepwise approach, each time incorporating the stakeholders listed above:
Step 1
Following the experts’ recommendation for a pilot programme, we held a large public engagement in 2021 to understand the community’s views toward the newborn genome programme. The community viewed the programme as favorable if it looked for treatable conditions in newborns, so only conditions that are early onset (none that present later in adulthood) and for which there is a treatment that needs to be started early in life. Once this public engagement was completed, the Minister of Health announced in 2021 the pilot programme's launch.
After the programme was funded last Fall, we gathered a working group to develop a framework for the conditions that would be treated. The committee included physicians, policymakers, scientists, patient group representatives, and members of the public. Over the course of nine months, this working group developed four principles to guide the types of conditions for which we would test:
Principle A: There is strong evidence that the genetic variant(s) causes the condition and can be reliably detected.
Principle B: A high proportion of individuals who have the genetic variant(s) would be expected to have symptoms that would have a debilitating impact on quality of life if left undiagnosed.
Principle C: Early or pre-symptomatic intervention for the condition has been shown to lead to substantially improved outcomes in children, compared to intervention after the onset of symptoms.
Principle D: Conditions screened for are only those for which the interventions are equitably accessible for all.
The group then conducted a series of focus groups with people from the public plus an online survey to understand the public’s perceptions of the principles and adjusted the principles based on this feedback. These four principles have now been widely vetted and are accepted by the NHS, physicians, and the public.
Step 2
The next step is to apply the four principles to each of the 700+ possible conditions to identify those that fit the framework and then sense-check this list of conditions with the physicians participating in the programme.
Beyond the list of conditions, we also need to develop a list of the genetic variants that are pathogenic for each disease gene. These will be the variants we research and on which we report. We are currently working on collating the list of known pathogenic variants from laboratories in the US and the UK.
While we will only report on the pre-defined pathogenic variants on this list, we will keep a record of all genetic variants identified to support the follow-up analysis on whether a condition ultimately developed or not in the child.
Step 3
Once we have the principles and the conditions approved by families and physicians, we will go to the NHS to ensure willingness and capacity to provide care for all conditions in the programme. This step is particularly important considering Principle D, which establishes that treatment for the conditions screened needs to be available to everyone in England. This also means that treatment needs to be approved for use in the UK. As part of the pilot, we will not consider conditions where only an experimental treatment (treatment undergoing testing in clinical trials) is available.
Step 4
Once we have the principles and the conditions, we will run our research plan by the Research Ethics Board and identify the Trusts (i.e., hospital systems) that will participate in the programme. This will happen within the next few months. Once this is done, we can begin to recruit families to participate in the programme in the Fall.
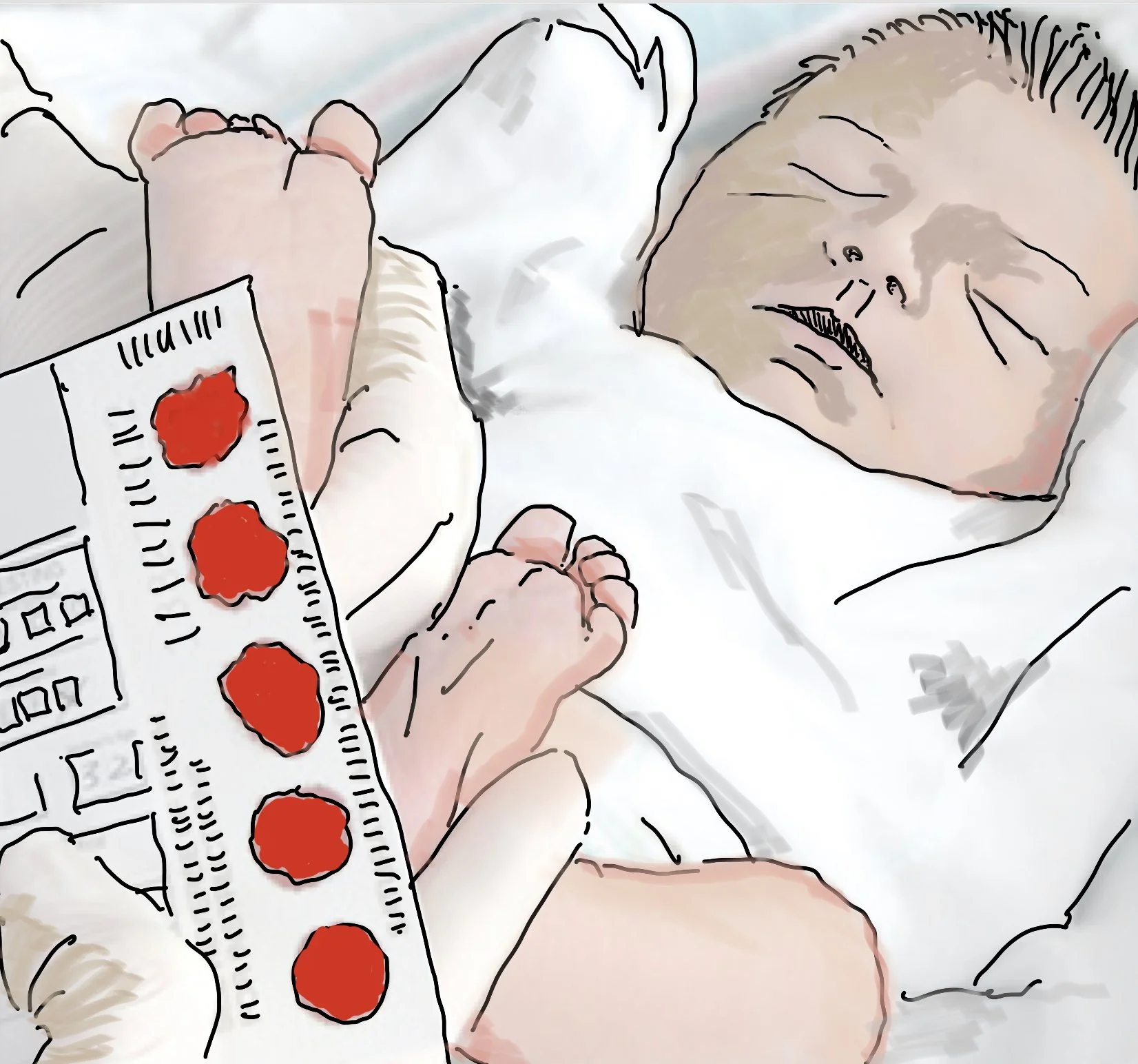
One key consideration as we embark on this project will be to make sure that we do not interfere with the current highly successful newborn screening program in the UK. We hope to use blood from the umbilical cord or a heel prick during day 0 of life. We are also considering a cheek swab on day 0 or day 5 (same day as the current NBS heel prick) in case we cannot obtain a blood sample on day 0 of life. We will plan the timing of our testing to deliver the results at 2 weeks of age. Any discrepancies with results from the current heel prick will go to the newborn screening lab to resolve before sending to the physician.
In Fall 2023, we anticipate recruiting parents in their third trimester of pregnancy through Trusts and beginning the informed consent process with these families. After this, we will take two years to collect data (2025-2026), followed by several years of follow-up. This follow-up period will serve to both understand how satisfied the parents were with the programme and to gather the necessary elements to do the economic analysis. As whole genome testing remains a screening procedure, we know that we will not find all the cases, and some children will still develop conditions we screened for but did not find. We anticipate that out of the 100,000 children we screen, about 500 will have a true positive, and perhaps 500 will have a false positive.
Once a screening comes back positive for a condition, this moves out of the domain of the research pilot and into normal clinical care. The next step will be to perform a diagnostic test to confirm the presence of the condition in the child and to begin treatment where appropriate. At this time, specialized genetic counseling will also be available to the parents, particularly in the context of future family planning.
How will this programme inform future clinical practice in the UK?
Through this pilot research programme, we hope to provide the NHS with the needed data to inform the decision about whether whole genome screening should be offered to every newborn in the country moving forward. There are three main goals our research will accomplish:
Find and treat – our first goal is to find children with treatable conditions through newborn screening and get them treated.
Develop research – our second goal is to conduct research to reliably identify more treatable conditions and improve detection and treatments for conditions that are currently not treatable.
Consider long-term use – our third goal, which is a bit more speculative, is to consider the possibility of the practical long-term use of genome mapping across a person's lifespan.
Looking at whole genome sequencing for newborn screening is not only being studied in the UK; there is a worldwide movement in this direction. Specialists such as Stephen Kingsmore, Wendy Chung, Robert Green, and Don Bailey are launching or have already launched programs in the US. In Belgium, Laurent Servais is leading a screening programme. Alessandra Ferlini is leading Screening4Care, a European Consortium programme. The Netherlands, Qatar, France, Australia, and China are also exploring the uses of whole genome screening. We are all working to find solutions to identify and treat conditions in the most efficient and streamlined way for the health of children everywhere.
Further reading on this programme:
About the interviewee
David Bick MD is the Principal Clinician for the Newborn Genomes Programme at Genomics England. Prior to his work in England, he was the Chief Medical Officer and a faculty investigator at the HudsonAlpha Institute for Biotechnology. Dr. Bick also served as the Medical Director of the Smith Family Clinic for Genomic Medicine located on the campus of HudsonAlpha Institute for Biotechnology and the Laboratory Director of the HudsonAlpha Clinical Services Laboratory.
He came to HudsonAlpha from the Medical College of Wisconsin where he was Professor in the Department of Pediatrics and the Department of Obstetrics & Gynecology at the Medical College of Wisconsin. At the Medical College of Wisconsin he was the Director of the Clinical Sequencing Laboratory, Director of the Advanced Genomics Laboratory at Children’s Hospital of Wisconsin, Medical Director of the Genetics Clinic at Children’s Hospital of Wisconsin, and Chief of the Division of Genetics in the Department of Pediatrics at Medical College of Wisconsin.
Dr. Bick received his medical degree from George Washington University School of Medicine in 1981 and completed his residency in Pediatrics at Yale-New Haven Hospital in New Haven, CT. At the Yale University School of Medicine, Dr. Bick completed a fellowship in Human Genetics and Pediatrics in 1986, followed by a post-doctoral research fellowship in Human Genetics in 1987. Dr. Bick is board certified in Pediatrics, Clinical Genetics, and Clinical Molecular Genetics.
He is a leader in the field of genomic medicine and has published numerous peer-reviewed articles, chapters, and reviews. Dr. Bick’s laboratories at the Medical College of Wisconsin and Children’s Hospital of Wisconsin were the first in the world to offer whole genome sequencing as a clinical test. He also developed the first Genomic Medicine Clinic in the United States.