Re-envisioning the Care Delivery Model in Saudi Arabia
This month's blog spotlights Saudi Arabia's ongoing work in reshaping its healthcare delivery model as a part of its Vision 2030 strategy. Dannah Al-Angari, Model of Care Learning Specialist, Ministry of Health, and I discuss the context behind this transformation, what the new model for healthcare delivery entails, and the expected outcomes of this effort.
Interview with Dannah Al-Angari
Why is Saudi Arabia changing its model for delivering care?
Transforming healthcare is a key part of the National Transformation Program under Saudi Arabia’s Vision 2030. The objectives are to increase access to health services across the kingdom and improve these services’ quality and efficiency. The transformation seeks to address the following challenges facing the Saudi Arabia population today:
““We commit ourselves to providing world-class government services which effectively and efficiently meet the needs of our citizens.””
Unhealthy lifestyle, increased prevalence of chronic conditions, and premature death – a high percentage of individuals in Saudi Arabia are overweight, and about ¾ of the population lack a regular checkpoint with the health system; chronic conditions, such as diabetes and hypertension are on the rise, and percentage of premature deaths from non-communicable diseases are much higher than in other developed countries
Increasing costs of care and inefficient health system navigation – many individuals do not currently have a clear understanding of how to navigate the healthcare system and at which points to engage with which levels of care
What does the healthcare transformation entail?
Care delivery in Saudi Arabia is being redesigned based on international best practices and trends. Key international drivers informing the development of the MoC were:
Value-based healthcare – shifting in focus from activity-based to outcome-based payments
Population health management – incentivizing preventing measures
Provider accountability – increasing autonomous and accountable care delivery
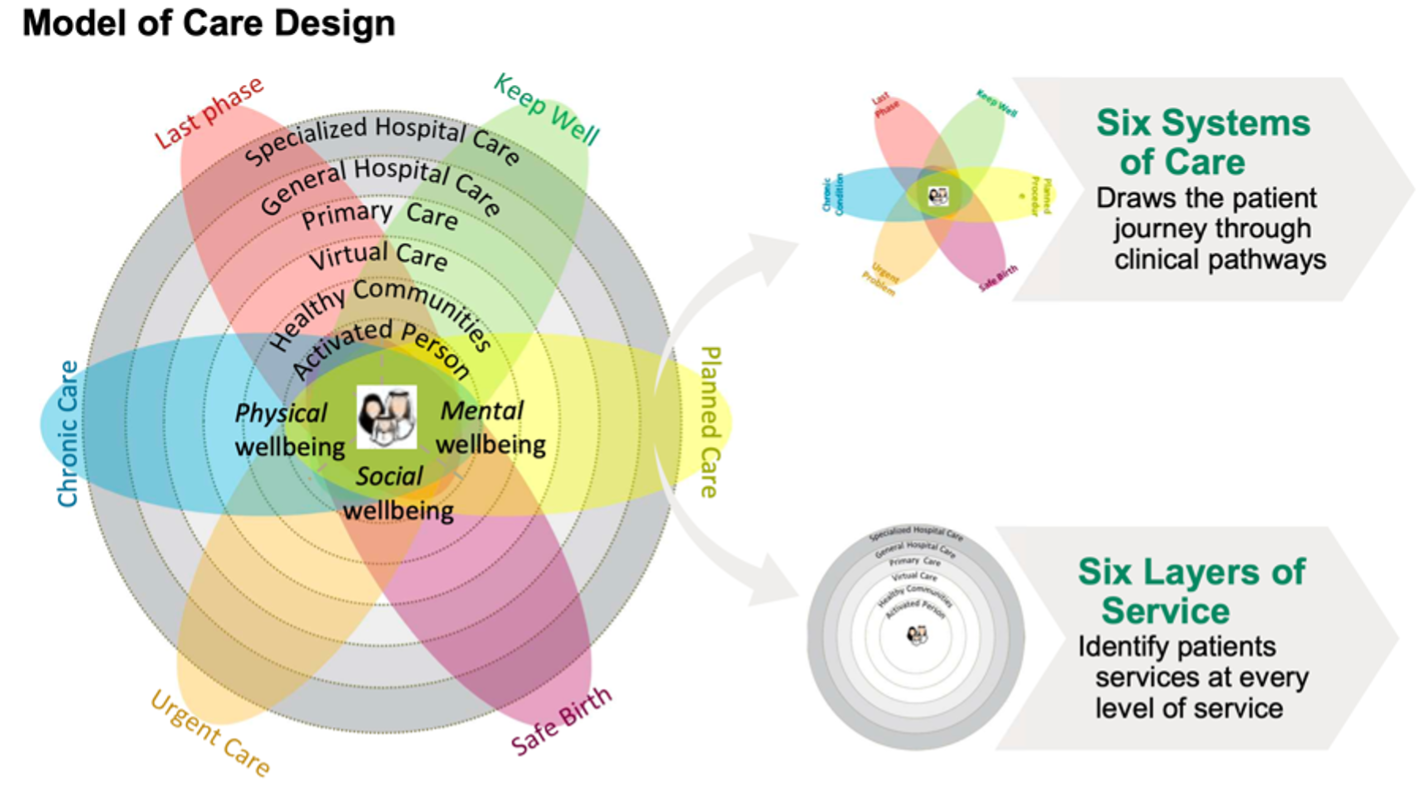
The new national Model of Care (MoC) comprises six systems of care, focusing on the different types of care the health system will deliver: preventative, planned, maternal and child, urgent, chronic, and palliative care. It is also composed of six layers of services, from empowering the individual to primary care and specialized health services. Each system of care establishes pathways for individuals to navigate care and has its measures of success.
Source: Saudi Arabia Ministry of Health
The MoC is further defined by 42 coordinated interventions aligned to either the system of care or cross-cutting across the systems. Examples of interventions aligned to systems of care include school wellness programs, length of hospital stay reduction initiatives, premarital and chronic disease screening, care coordination, and hospice care services. Examples of cross-cutting interventions include national guidelines, referral networks, outcomes monitoring, systemic data collection, and resource optimization.
The MoC will be delivered as follows:
A National Center of Excellence (CoE) – the CoE will provide national guidance, alignment, and standardization of frameworks and methodologies at a country level to streamline implementation of the MoC
Regional hubs – the hubs are part of regional business units that work to operationalize frameworks, ensure standardization, and advise and guide clusters in the implementation of the MoC in the region; the hubs also support capability building and offer a means for clusters to escalate issues
Local clusters – clusters are units of care delivery responsible for implementing all components of the MoC, improving pathways to care, and innovating at the local level; they are grouped into five geographical areas and supported by the corresponding regional hub
Clusters operate as separate entities; each cluster has independent governance and strategy setting. Under the new MoC, clusters are responsible for developing operational plans that prioritize the interventions most relevant to their local populations. Implementation of the transformation is currently underway; many clusters are either in the strategic planning and intervention prioritization phase or already moving to the operationalization of the MoC.
With the regional hubs’ support and oversight, the new system will encourage cross-learning at the local cluster and regional hub level through a repository of information and sharing of lessons learned and success stories. Regional hubs will also support capability building through training and coordination and provide advisory and guidance on the planning, design, and implementation of the MoC.
The healthcare system’s transformation also includes restructuring how care is covered and financed, placing emphasis on outcome-based payment structures, and engendering amicable competition between clusters to improve care for all.
What benefits are expected from the implementation of the new Model of Care?
Specific outcomes expected from the transformation include improved access to health services across the nation; aligned service offerings at all levels of care; enabled tracking of outcomes to monitor services and improve quality; empowered individuals with an understanding of individual care pathways to navigate the system. Ensuring the mental, physical, and social wellbeing of the individual is central to the MoC model.
Overall, the healthcare transformation effort is expected to improve health, healthcare, and value for all across Saudi Arabia.
You can learn more about Saudi Arabia’s Healthcare Transformation Strategy by clicking below.
About the interviewee
Dannah Al-Angari, MPH works as a Learning Specialist in a Saudi Arabia Ministry of Health subsidiary since April 2020. As part of her role, she organizes and coordinates initiatives including leadership training for primary health care centers in Saudi’s Eastern province. She also pioneered the Imam Abdulrahman bin Faisal Public Health Internship Program, which she oversees in her role.
Dannah’s received her Bachelor’s degree from the University of Washington with a double major in Public Health and Physiology, and her MPH in Health Policy and Management from Columbia University.